Climate Change Undermines Healthy Aging
Climate change poses unique and dangerous risks for older people, especially those experiencing cognitive challenges.

Members of U.S. Coast Guard rescue an elderly woman along with her husband and their pets after their home was flooded by Hurricane Florence, in Brunswick County, North Carolina, on September 16, 2018.
Petty Officer 3rd Class Trevor Lilburn/U.S. Coast Guard
Co-authored with Prof. Megan Zuelsdorff (School of Nursing, University of Wisconsin-Madison)
The accumulation of heat-trapping climate pollution in the Earth’s atmosphere from burning fossil fuels is continuing to push humanity down a dangerous path. In recent years, the world’s leading public health voices have sounded the climate alarm as an emergency because a wide array of dangerous climate threats—including stronger heatwaves, wildfires, and coastal storms—are intensifying, with a ferocity that is life-threatening in many cases. A collection of research articles just published in a special issue of a leading scientific journal on aging, The Gerontologist, sheds new light on the intersections of climate and demographic trends and identifies mechanisms by which climate change will likely undermine healthy aging globally. This research also underscores a growing evidence base on how actions to slow climate disruption and improve community preparedness can also help to promote healthier and safer aging.
Climate Risks to Healthy Aging
Authoritative voices including the recent Fifth U.S. National Climate Assessment have drawn attention to the disproportionate burden of climate threats on vulnerable populations, including the very young, older folks, low-income communities, and racial and ethnic minorities. The climate problem is intensifying already severe health disparities in older populations living in the U.S. and beyond, in part due to intersecting threats related to climate exposures, sensitivity factors like pre-existing health conditions, and a lack of access to health-protective resources and affordable medical care.
While a full accounting of the true toll of climate change on human health remains challenging to assemble, the available data are sobering in describing the recent deaths, illnesses, and injuries linked to climate-sensitive threats. At the same time, the global population is aging, with a near-doubling of the age 60+ population expected between 2015 and 2050. But these risks are not just a future worry, they’re a present-day threat. A 2019 study by experts at NRDC and the University of California-San Francisco, identified hundreds of deaths and tens of thousands of emergency room visits and hospitalizations related to a small sample of recent climate-sensitive events across the U.S.—with the highest financial burden of those health harms shouldered by Medicare patients (a government-administered program for people aged 65 and older which covers more than 60 million individuals) and people covered under Medicaid. But due to a lack of adequate public health surveillance, our visibility into how climate change threatens older populations remains limited.
Unique Challenges for Dementia Patients
The new special issue of The Gerontologist signals the next phase in an ongoing effort to address this evidence gap through a set of research articles on the complex intersections between climate change impacts and the science of aging. In an article co-authored with Professor Megan Zuelsdorff at the University of Wisconsin-Madison, we propose a new framework for connecting the dots between climate risks and the burden of Alzheimer’s Disease and Related Dementias (ADRD). ADRD, an umbrella term used to describe a set of debilitating conditions that impair memory, thought processes, and functioning, primarily among older adults. ADRD is already a significant global challenge, with more than twice as many people living with these devastating conditions in 2019 as there were in 1990.
In addition to those individuals directly impacted by ADRD, the diagnosis typically triggers a complex and intense cascade of emotional, logistical, and financial challenges for families and caregivers. While research into the modifiable risk factors that contribute to ADRD incidence has gained ground over the years, there is still no widely effective treatment or cure that could reverse or fully stall ADRD progression once it begins. To date, most of the research on climate and ADRD has focused on the role of outdoor air pollution (in the U.S., a large share generated from burning fossil fuels) in contributing to inflammation that can heighten a person’s risk of developing dementia.
Unfortunately, the intensifying climate crisis is poised to exacerbate the current and future experience of ADRD because of an array of social and physical and environmental stressors that are intensifying all around us. In our article, we propose a new framework that connects the dots between climate change stressors like extreme heat and wildfires and the different kinds of settings that shape ADRD risk profiles, including housing and infrastructure, social environments and community resources, individual experiences, and biological processes happening inside the body:
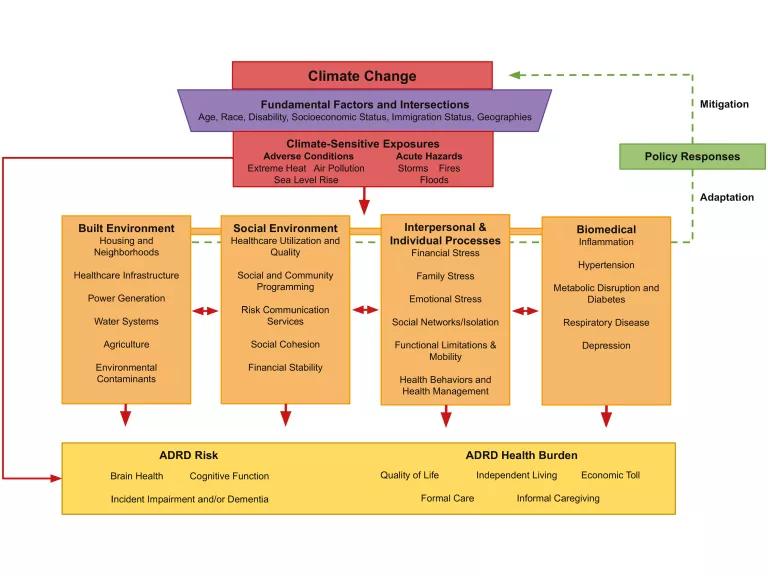
Framework depicting how climate-sensitive exposures affect risk and health burden of Alzheimer’s disease and related dementias.
Zuelsdorff and Limaye (2023)
While prior scientific work has linked a number of biological, social, and environmental factors to ADRD risks, few studies have considered how climate change-related disruptions to human and natural systems are changing these complex risk profiles. For example, climate change-worsened hazards such as coastal storms and wildfires are known to cause stressful and rushed evacuations for individuals and families in harm’s way. Unfortunately, acute and chronic stress taxes the body and the brain; stressful life events have been shown to elevate one’s risk for cognitive impairment later in life.
Climate Actions Can Reduce Dementia Risks
While it is clear from our review of the available evidence that climate change poses a major obstacle to healthy aging and reduction in the ADRD burden, there is good news. Because the same fossil fuels that are causing climate havoc are also spewing harmful air pollution that harms older people disproportionately, a transition away from these polluting energy sources towards cleaner, healthier options (such as solar power and wind energy) can deliver benefits for our health and the climate. But because of the scale of climate pollution that we’ve already added to the Earth’s atmosphere, we must also better prepare our communities for the climate hazards that we will continue to face in future years.
These adaptation strategies can take many forms, and our article provides examples of measures that can address populations living with ADRD and those at risk of developing dementia. We must adapt our built and social environments to better enable healthy aging through a wide range of efforts such as publicly-available cooling centers and clean air shelters, social programming to connect older adults to supportive resources during disasters, and energy subsidies, building codes, and indoor heat standards that can provide relief for older people from searing heat outside and inside the home. Early warning systems (like those for extreme hat wildfire smoke risks) and transportation networks should take into account the unique needs of seniors, including many who may not be reached by smartphone- or internet-based communication modes.
At a broader level, the healthcare facilities and caregiving resources that ADRD-affected individuals and families rely on should expanded to consider climate threats. Hospitals and emergency rooms need climate adaptation plans that can help to provide continuity of care during hazardous events. As our article points out, healthcare practitioners are well-situated to help caregivers anticipate and plan for climate threats. But in order for health professionals to deliver on that opportunity and better prepare their older patients, we need to strengthen and expand climate-related training and support resources. Many such efforts are currently underway, including projects to organize and embed climate information in health professional curricula, show medical experts how to better characterize climate-related harms in patient chart data, and reach older populations with climate and health information tailored to meet their unique needs and perspectives.
Aging on a Warming Planet
While the national attention span may shift rapidly from one climate-related disaster to the next, the less obvious and slower-to-develop health consequences set into motion by these events, including ADRD, are obscured in the available data and thus difficult for medical experts and policymakers to grasp. A framework like ours can help to uncover these linkages and draw attention to the ways in which dementia risks could worsen in a warming and aging world—and how climate action can help us to address these worrying trends. While scientists and researchers work to paint a fuller picture of the threats older populations face from climate change, the available evidence is more than enough to motivate climate change mitigation and adaptation policies and investments that can help promote healthier and safer aging.




